62-66 Clinical rheumatology. 1996, 15. Suppl. 1
The Use of a Low Starch Diet in the Treatment of Patients Suffering from Ankylosing Spondylitis
A. EBRINGER*, C. WILSON'**
* Immunology Section, Division of Life Sciences. King's College. London.
* * Department of Rheumatology, UCL School of Medicine, Middlesex Hospital. London, England.
Summary The majority of ankylosing spondylitis (AS) patients not only possess HLA-B27, but during active phases of the disease have elevated levels of total serum IgA, suggesting that a microbe from the bowel flora is acting across the gut mucosa.
Biochemical studies have revealed that Klebsiella bacteria, not only possess 2 molecules carrying sequences resembling HLA-B27 but increased quantities of such microbes are found in fecal samples obtained from AS patients and such patients have Crohn's like lesions in the ileo-caecal regions of the gut. Furthermore AS patients from 10 different countries have been found to have elevated levels of specific antibodies against Klebsiella bacteria. It has been suggested that these Klebsiella microbes, found in the bowel flora, might be the trigger factors in this disease and therefore reduction in the size of the bowel flora could be of benefit in the treatment of AS patients.
Microbes from the bowel flora depend on dietary starch for their growth and therefore a reduction in starch intake might be beneficial in AS patients. A "low starch diet" involving a reduced intake of "bread, potatoes, cakes and pasta" has been devised and tested in healthy control subjects and AS patients. The "low starch diet" leads to a reduction of total serum IgA in both healthy controls as well as patients, and furthermore to a decrease in inflammation and symptoms in the AS patients.
The role of a "low starch diet" in the management of AS requires further evaluation.
Key words Ankylosing spondylitis, Low Starch Diet, Treatment of AS.
INTRODUCTION
The discovery that the majority of patients with ankylosing spondylitis (AS) are HLA-B27 positive has led to a search of suitable biochemical models which could explain the association, the two most important being the "receptor theory" and the "molecular mimicry theory" (1). Using the "molecular mimicry theory" as a model, 2 molecules have been identified in Klebsiella microorganisms, which possess sequences resembling HLA-B27 (2,3). Furthermore AS patients from 10 different countries have been found to have elevated levels of specific antibodies against Klebsiella microorganisms (4) and it has been suggested that these microbes are probably the causative agents of this disease (5). These observations could be of relevance in the treatment and even prevention of this condition.
SERUM IgA AND THE INVOLVEMENT OF THE GUT IN AS
Elevated levels of total serum IgA are found in AS patients during active phases of the disease (6,7) and this correlates with elevations in acute phase reactants such as erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP), as well as with increased isolation of Klebsiella microbes from fecal samples (8). Furthermore ileo-colonoscopic studies from Ghent in Belgium, have revealed that during active phases of the disease, over 50% of AS patients have microscopic Crohn's like lesions in the gut mucosa (9).
Clearly gut involvement is present during active phases of the disease in AS patients and the most likely trigger factor would appear to be Klebsiella bacteria found in the bowel flora. Thus one possible way of treating relapses or acute phases of the disease in AS could be by reducing the number of microorganisms in the bowel flora, including Klebsiella. The main source of substrates on which colonic microbes depend are the residual dietary nutrients entering the large bowel following incomplete digestion.
STARCH AS THE SOURCE OF THE MAIN BACTERIAL SUBSTRATE IN THE GUT
Early studies in patients with AS using low doses of antibiotics such as co-trimoxazole and phthalyl-sulphathiazole did not lead to any significant improvements, although some patients admitted that the use of antibiotics decreased the dose of "nonsteroidal anti-inflammatory drugs" (NSAID's) required to control their symptoms.
A. CARBOHYDRATES AND THE GROWTH OF KLEBSIELLA
In 1982 an AS patient was placed on a low residue diet for weight reasons and 4 months later when he was reviewed in the outpatient AS clinic, he pointed out, that not only had he lost weight but his backache had gone. A review of the literature showed that subjects on low carbohydrate diets have low levels of Klebsiella microorganisms in their stools. Faecal bacterial studies were carried out on 47 subjects on a high carbohydrate/low protein diet and compared to 45 subjects on a low carbohydrate/high protein diet. The mean number of Klebsiella microorganisms in the "high carbohydrate group" was 30,000 per gram of faeces compared to a value of 700 per gram of faeces in the "low carbohydrate group" (10).
The substrates available in the gut for fermentation are one of the major factors in determining the microbial population in the various regions of the gastrointestinal tract. These substrates include simple sugars, polysaccharides such as starch or cellulose, proteins, peptides, fats and other lipids. Klebsiella microbes do not grow on cellulose derived from plants (11) but can readily grow on simple sugars. Equal amounts (5 G/L) of simple sugars and amino acids were compared for their ability to act as nutrients for the growth of Klebsiella pneumoniae in 24 hour cultures and the number of bacteria obtained compared for the different simple substrates.
The mean number of Klebsiella microbes for 3 different sugars (glucose, sucrose and lactose) per gram of substrate was 8.7 ± 1.0 (mean ± SE) (x 109) (p<0.001) compared to a value of 0.8 ± 0.2 (x 109) obtained following incubation with 11 different amino acids (12). Thus Klebsiella microorganisms grow better on carbohydrate than on protein substrates.
B. ILEOSTOMY AND ORAL HYDROGEN STUDIES
One way of finding out which substrates are available for bacterial fermentation in the ileo-caecal region, which is the main site of microscopic lesions, is to analyze ileostomy fluid obtained from patients whose colon has been removed surgically. In a study of 26 ulcerative colitis patients, who had undergone proctocolectomy with ileostomy, it was found that the "ileostomy fluid" contained significant amounts (5-10 G/D) of mono- and disaccha-rides (13).
The source of these carbohydrates could be dietary starch. Nearly all normal subjects fail to absorb appreciable amounts (5 - 20%) of starch in wheat flour, commonly present in bread and pasta, as assessed by oral hydrogen excretion studies, following a test meal. This is due to the formation of insoluble complexes between some carbohydrate and protein components of wheat. Breath hydrogen concentrations were measured for 5 hours after an overnight fast, followed by a test meal containing equal amounts of either sucrose or bread/pasta. The sucrose meal produced no increase in oral hydrogen but significant amounts were detected at 4 and 5 hours after a test meal with either bread or pasta (14).
It would appear that dietary mono- and disaccharides can be readily absorbed in the stomach and upper part of the small bowel and therefore they are not available as substrates for bacterial fermentation in the colon. The carbohydrates detected in the "ileostomy fluids" would appear to be derived from complex carbohydrates. These observations could form the basis of a "low starch" diet for AS patients.
COMPOSITION OF "LOW STARCH DIET"
The carbohydrates detected in the "ileostomy fluids" would appear to be derived from starch present in flour and potatoes. Therefore an exclusion diet removing complex carbohydrates such as starch but not simple carbohydrates such as dietary glucose and sucrose might inhibit the growth of Klebsiella and therefore could affect disease activity in patients with AS.
A simple "low carbohydrate diet" was devised, the main emphasis being in advising AS patients to significantly reduce their intake of "bread, potatoes, cakes and pasta". (Table). To compensate for the calorie loss incurred by reducing starch intake, subjects were advised to in crease their intake of
Table I: List of common foods whose intake was to be increased or decreased by the AS patients in an endeavour to achieve a "low starch diet".
Increase |
Reduce |
Red Meat |
Bread |
White Meat |
Potatoes |
Fish |
Chips |
Beans & Peas |
Rice |
Nuts |
Spaghetti |
Vegetables & Salads |
Cereals |
Milk |
Cakes |
Fruit |
Biscuits |
meat, fish, fruits and vegetables, but excluding potatoes.
Diet sheets were prepared which were given to the patients together with a short summary of why such a "low starch diet" might benefit the AS patients: "It was pointed out that the great majority of AS patients carried HLA-B27 and this marker was thought to resemble some molecules present in Klebsiella microbes. The majority of AS patients had antibodies to these microbes and they appeared to grow on substrates derived from dietary starch. It was emphasized that this interpretation was controversial but no harm would occur if they tried the diet, especially if this led to a reduction of NSAID's, which all patients were aware, caused many undesirable side-effects. They were free to modify or go off the diet at will."
The diet was tried in 2 groups of healthy subjects before studies were carried in AS patients.
1. Open study with 21 healthy subjects
A group of 21 healthy subjects (University students and hospital staff) attempted the "low starch diet" for a period of 8 weeks. The mean serum IgA significantly dropped from 255 mg/dl at the start of the study to 212 mg/dl (p -< 0.001) by the end of 8 weeks.
2. Nutritionally controlled study with 11 healthy subjects
In the second study, 39 healthy volunteers were recruited from Town Hall staff, local police and University students. All underwent a one-week measured food intake monitored by a qualified nutritionist and serum IgA were measured at the end of the first week: 11 individuals were found to have serum IgA in excess of 250 mg/dl. They undertook a 5-week "low starch diet" with a mean starch reduction of 40%. Each individual received a personal "iso-calorie, low starch diet" proto col, which was determined from their one-week measured food intake study. Mono- and disaccharides such as sucrose were not restricted and a list of appropriate "starch exchangers" was provided. The mean serum IgA fell from an initial level of 388 mg/dl at the start of the diet to 259 mg/dl (p < 0.001) at the end of the 5-week period.
These 2 studies in healthy individuals, clearly show that serum IgA can be controlled by the dietary intake of starch. Since elevated levels of serum IgA are known to occur in AS patients, a similar approach might produce not only a drop in serum IgA but possibly affect disease activity, as measured by acute phase reactants or even lead to clinical improvements.
LOW STARCH DIET IN AS PATIENTSIn an initial study of 36 active AS patients (ESR> 15 mm/hr), the mean ESR dropped from 38 ± 3 mm/hr (mean ± SE) to 24 ± 2 mm/hr (p ·< 0.001), when studied over a period of 9 months, but no such difference was observed in the same group of patients when examined retrospectively for the same period of time before they went on the "low starch diet" (12). A significant drop in total serum IgA was also observed in these patients over this period.
The majority of these AS patients reported that the severity of their symptoms declined and in some cases completely disappeared. Many patients noticed that their requirement of NSAID's also decreased.
Since 1983, the "low starch diet" has been used in the treatment of over 450 AS patients attending the "AS Clinic" at the Middlesex Hospital in London. Over half of these patients do not require any medication and are treated by diet alone.
The remaining patients, may require low doses of NSAID's and those with an ESR elevation above 20 mm/ hr are treated with sulphasalazine-EN (Salazopyrin), in the dose range from 0.5 G to 3.0 G daily. Another advantage of the "low starch diet" is that lower doses of sulphasalazine-EN are required to achieve a therapeutic effect, thereby avoiding some of the undesirable side-effects of NSAID's.
It takes some time, usually 3 to 6 months for the patients to become familiar with the "low starch diet". Patients are advised to consult the members of the AS Clinic, either the attending physician or specially trained nursing staff. The AS patients are encouraged to ring the sister in charge of the AS Clinic, with any queries regarding the management of their condition and especially to discuss any problems associated with the "low starch diet". A minority of patients find the diet difficult to adhere to and then they have to be treated with higher doses of NSAID's.
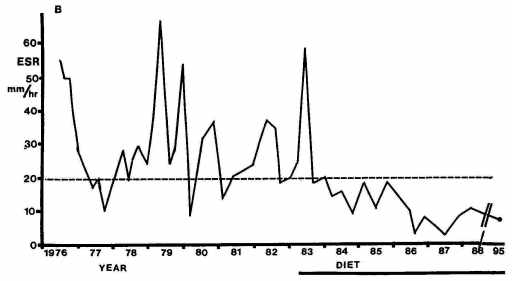
Fig. Enthrocyte sedimentation rate (ESR mm/hr) in patient B from 1976 to 1995.
Case
Mrs. B, who is HLA-B27 positive, had her first symptoms of AS in 1969, when she was 20 years old. She was first seen in the "AS Clinic" in 1976 and over the subsequent 7 years had almost continuous, unremitting pains affecting large peripheral joints, thoracic cage and the whole of the spinal column, eventually leading to complete ankylosis. During this period, her ESR was rarely below 20 mm/hr and she acquired the radiological and clinical stigmata of advanced AS. She started on the "low starch diet" in 1983 and her clinical condition improved over the subsequent months. Her ESR dropped to below 20 mm/hr and has remained normal for the last 12 years. She was last seen in May 1995 when her ESR was 5 mm/hr and her haemoglobin was 13.2 G/dl. She takes an occasional NSAID tablet for the mechanical pains produced by her rigid spine. (Figure)
Clearly the use of a "low starch diet" in the treatment of AS patients during active phases of the disease could be beneficial but these results must be evaluated by prospective, longitudinal studies.
TREATMENT OF AS PATIENTS AND HLA-B27
The discovery of the association of HLA-B27 with AS has opened new approaches to the treatment of this disease which will require evaluation by many rheumatological centers in different countries.
The "molecular mimicry theory" has led to the recognition that Klebsiella microorganisms are somehow involved in this disease.
Several independent studies have demonstrated that sulphasalazine is an effective drug in the treatment of AS and it is known that this drug has antibiotic activity against Klebsiella microorganisms. Furthermore, Finnish studies have demonstrated that following treatment with sulphasalazine, the titre of anti-Klebsiella antibodies decreases (15).
Another possible therapeutic approach is to restrict the growth of gut Klebsiella by a modified "low starch diet".
Rheumatological centres can now contribute to the debate as to the role of HLA-B27 in AS, by studying the response of patients following treatment with anti-bacterial antibiotics and diet manipulation.
CONCLUSION
The role of a "low starch diet" and anti-Klebsiella therapy needs to be evaluated in AS patients.
Acknowledgements: This study was supported by the Trustees of the Middlesex Hospital
1. Ebringer, A. Theoretical models to explain the association of HLA-B27 with ankylosing spondylitis. Scand J Rheumatol 1990, sup 87,151-163.Correspondence to: Dr. Alan EBRINGER,
Division of Life Sciences, King's College, Campden Hill Road, Kensington, LONDON W8 7AH, U.K.